diverticulitis
Diverticulitis is a common digestive condition that can lead to significant discomfort and complications if left untreated. Understanding its causes, symptoms, and treatment options is crucial for managing the condition effectively. This article delves into everything you need to know about diverticulitis, providing a comprehensive guide to its diagnosis and care.
Table of Contents
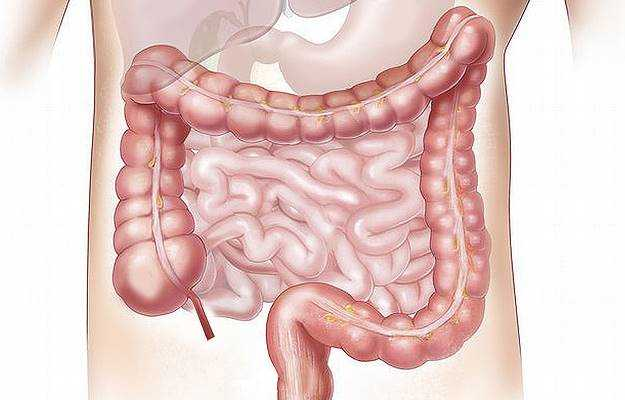
What Is Diverticulitis?
Diverticulitis occurs when small pouches, known as diverticula, that form in the lining of the colon become inflamed or infected. These pouches are more common as people age and may not cause symptoms unless they become problematic.
Diverticulosis vs. Diverticulitis
- Diverticulosis: The presence of diverticula without any associated inflammation or symptoms.
- Diverticulitis: The inflammation or infection of diverticula, leading to pain and other symptoms.
Causes of Diverticulitis
Understanding the underlying causes of diverticulitis can help in prevention and early detection.
Weak Spots in the Colon Wall
Diverticula form when weak spots in the colon wall bulge outward under pressure, often due to:
- Chronic constipation
- Straining during bowel movements
- Low-fiber diets
Inflammation and Infection
When waste material or bacteria get trapped in diverticula, it can lead to inflammation or infection, causing diverticulitis.
Risk Factors
Certain factors increase the likelihood of developing diverticulitis:
- Age: Risk increases with age, particularly after 40.
- Diet: Low fiber intake and high consumption of processed foods can contribute.
- Lifestyle: Sedentary habits and obesity are linked to higher risks.
- Smoking: Smokers are more likely to develop complications.
- Medications: Long-term use of NSAIDs, steroids, or opioids may play a role.
Symptoms of Diverticulitis
Symptoms can range from mild discomfort to severe complications.
Common Symptoms
- Abdominal Pain: Often localized to the lower left side of the abdomen.
- Fever: A sign of infection or inflammation.
- Changes in Bowel Habits: Diarrhea or constipation.
- Nausea and Vomiting: May occur due to intestinal irritation.
- Bloating: A feeling of fullness or discomfort in the abdomen.
Severe Symptoms
In some cases, diverticulitis may lead to:
- Persistent pain
- Blood in stool
- Peritonitis (inflammation of the abdominal lining)
- Abscesses or fistulas
How Is Diverticulitis Diagnosed?
Diagnosing diverticulitis involves a combination of clinical evaluation and diagnostic tests.
Medical History and Physical Exam
A healthcare provider may:
- Assess symptoms and medical history.
- Perform a physical examination, focusing on the abdomen.
Diagnostic Tests
- Blood Tests: To check for infection or inflammation.
- CT Scan: The most common imaging test to confirm diverticulitis and assess complications.
- Colonoscopy: Typically performed after the acute phase to evaluate the colon.
Treatment Options for Diverticulitis
The treatment approach depends on the severity of the condition.
Mild Cases
- Dietary Modifications: Switching to a liquid or low-fiber diet to allow the colon to heal.
- Antibiotics: Prescribed to treat infections.
Severe Cases
- Hospitalization: May be necessary for intravenous antibiotics and fluids.
- Surgery: Required in cases of recurrent diverticulitis or complications such as abscesses or perforations.
Preventing Diverticulitis
Prevention focuses on maintaining a healthy digestive system.
Dietary Tips
- Increase Fiber Intake: Aim for 25-30 grams of fiber daily from fruits, vegetables, whole grains, and legumes.
- Stay Hydrated: Drink plenty of water to aid digestion.
- Limit Red Meat: Excessive consumption may increase the risk.
Lifestyle Changes
- Regular Exercise: Helps maintain bowel health.
- Avoid Smoking: Reduces the risk of complications.
- Maintain a Healthy Weight: Prevents added pressure on the colon.
Potential Complications of Diverticulitis
If untreated, diverticulitis can lead to serious complications.
Common Complications
- Abscess Formation: Pockets of pus in the colon.
- Perforation: A hole in the colon wall, leading to peritonitis.
- Bowel Obstruction: Narrowing of the colon due to scarring.
- Fistulas: Abnormal connections between organs.
When to See a Doctor
Seek medical attention if you experience:
- Persistent abdominal pain
- Fever not responding to medication
- Severe constipation or diarrhea
- Blood in stool
Living with Diverticulitis
Managing diverticulitis involves a combination of medical care and lifestyle adjustments.
Long-Term Management
- Regular check-ups to monitor the condition.
- Adhering to dietary and lifestyle recommendations.
- Being vigilant for signs of recurrence or complications.
Emotional and Mental Health
Chronic conditions can take a toll on mental health. Consider joining support groups or seeking counseling if needed.
FAQs About Diverticulitis
Can Diverticulitis Be Cured?
While diverticula cannot be reversed, symptoms of diverticulitis can be managed effectively with proper treatment.
Is Surgery Always Necessary?
No, most cases are treated with medication and lifestyle changes. Surgery is reserved for severe or recurrent cases.
What Foods Should I Avoid?
During an active episode, avoid nuts, seeds, and high-fiber foods. Once healed, focus on a balanced, high-fiber diet.
Conclusion
Diverticulitis is a manageable condition with the right approach to treatment and lifestyle. By recognizing the symptoms early and making necessary changes to diet and activity levels, individuals can lead a healthy, symptom-free life. If you suspect you have diverticulitis, consult a healthcare provider promptly for accurate diagnosis and effective care.